Board-Certified Plastic Surgeons Serving Denver & Lone Tree, Colorado
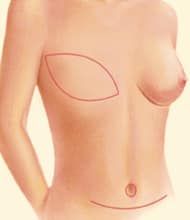
Breast reconstruction is a deeply personal decision for women affected by breast cancer or other conditions. Autologous breast reconstruction uses your own tissue and cells for a natural approach.
At Park Meadows Cosmetic Surgery in Lone Tree, Colorado, our board-certified plastic surgeons specialize in advanced breast reconstruction techniques, serving women in Denver, Highlands Ranch, and surrounding areas.
Read about the techniques our plastic and reconstructive surgeons can use to perform breast reconstruction using your own cells and tissue.
What Is Autologous Breast Reconstruction?
Autologous breast reconstruction uses skin, fat, and sometimes muscle from another part of your body to rebuild your breast. As opposed to implant-based reconstruction, this approach provides long-lasting results without using synthetic materials.
Types of Autologous Breast Reconstruction
We offer multiple types of autologous breast reconstruction, including the following:
- DIEP Flap: A muscle-sparing option that uses abdominal skin and fat while preserving the abdominal muscles.
- SIEA Flap: An even less invasive alternative to the DIEP Flap, avoiding disruption of abdominal muscles entirely.
- SGAP Flap: Utilizes skin and fat from the buttocks for reconstruction without involving muscle.
- TUG Flap: Uses tissue from the upper inner thighs, offering the added benefit of an inner thigh lift.
- Latissimus Flap: Relies on skin, fat, and muscle from the back, often combined with an implant for added volume.

Read about each type of autologous breast reconstruction method in more detail below.



DIEP Flap
The Deep Inferior Epigastric Perforator (DIEP) Flap is a muscle-sparing breast reconstruction technique that uses skin and fat from the abdomen, similar to tissue removed during a tummy tuck, without damaging the abdominal muscles.
Key Benefits
- Muscle Preservation: Unlike the TRAM Flap, the DIEP Flap spares the rectus abdominis muscle, reducing recovery time and long-term weakness.
- Natural Reconstruction: Skin and fat from the abdomen are transferred to the chest to create a natural-looking breast.
- Nerve Reconstruction: This procedure offers the possibility of reconnecting nerves to restore sensation to the breast skin.
Important Details
- The surgery requires highly skilled techniques and is performed by only a small number of surgeons nationwide.
- Preserving abdominal muscles helps improve recovery and minimize complications.
- Silicone scar therapy can be used to reduce the appearance of scars.
The DIEP Flap is the preferred method at The Breast Center at Park Meadows Cosmetic Surgery, offering advanced reconstruction with optimal results.

SIEA Flap
The Superficial Inferior Epigastric Artery (SIEA) Flap is similar to the DIEP Flap but even less invasive. This procedure uses skin and fat from the abdomen for breast reconstruction without entering or disturbing the abdominal muscles, making it the closest option to a true "tummy tuck."
Key Benefits
- Muscle Preservation: The abdominal muscles remain completely undisturbed, further reducing recovery time and risk of complications.
- Minimally Invasive: Because the artery and vein lie superficial to the muscle, there is no need to dissect through it.
Important Details
- Only ten to twenty percent of patients have the anatomy needed for this procedure, where the artery and vein are large enough to support reconstruction.
- If you are an ideal candidate, the surgeons at Park Meadows Cosmetic Surgery can use this approach to minimize the impact on the abdominal wall even further.
The SIEA Flap offers an advanced, muscle-sparing solution for breast reconstruction, providing natural results with reduced disruption to the donor site.
SGAP Flap
The Superior Gluteal Artery Perforator (SGAP) Flap is a microsurgical breast reconstruction technique that uses skin and fat from the buttock, supplied by the superior gluteal artery. This procedure does not involve muscle, making it a muscle-sparing option for women with limited donor tissue in other areas.
Key Benefits
- Muscle-Sparing: Only skin and fat are used, preserving the gluteal muscles.
- Donor Site: Suitable for women with limited tissue in the abdomen or other common donor sites.
Important Details
- The procedure is highly specialized, and even fewer surgeons perform SGAP Flaps than DIEP Flaps.
- The operation leaves a permanent scar across the buttock, typically hidden under bikinis or full-cut underwear.
- Most surgeons perform one SGAP at a time; bilateral reconstructions are only attempted by a handful of surgical teams.
The SGAP Flap is a valuable option for women seeking autologous breast reconstruction with their own tissue while preserving muscle at the donor site.
TUG Flap
The Transverse Upper Gracilis (TUG) Flap is an innovative breast reconstruction technique for women with limited traditional donor sites. This procedure uses skin and fat from the upper inner thigh, providing excellent tissue for reconstruction and offering the additional benefit of an inner thigh lift.
Key Benefits
- Dual Purpose: Reconstructs the breast while reshaping the inner thigh.
- Bilateral Reconstruction: Both breasts can be reconstructed in a single surgery.
Important Details
- The scars run along the groin crease and are typically hidden by underwear or swimwear.
- This is a newer method, performed by only a few highly skilled surgeons in the United States and Canada.
- Few plastic surgeons are familiar with or trained in this technique.
The TUG Flap is an excellent option for women considering autologous reconstruction who also have excess tissue in the thighs, offering natural results and additional aesthetic benefits.
Latissimus Flap
Latissimus Flap The Latissimus Flap is an older breast reconstruction technique that uses skin, fat, and the latissimus muscle from the back. This pedicled flap remains a valuable option in certain cases. Key Benefits Alternative Donor Site: Suitable for patients with limited abdominal tissue or as a backup option for challenging reconstructions. Important Details This technique sacrifices a large muscle to maintain blood supply to the transferred tissue. It often requires the addition of a breast implant to achieve the desired breast size. The Latissimus Flap is most often used as a secondary option or for patients with limited donor site availability.
Benefits of Autologous Breast Reconstruction
Autologous breast reconstruction offers several advantages for women seeking a natural and personalized approach to rebuilding their breasts:
- Natural Appearance and Feel: Tissue from your own body mimics the look and feel of a natural breast more closely than implants.
- Long-Lasting Results: Since no synthetic materials are used, the reconstructed breast ages naturally with your body.
- No Risk of Implant Complications: Avoids risks such as implant rupture, capsular contracture, or the need for replacement surgeries.
- Improved Symmetry: Can create a better match with the remaining breast in terms of shape and size.
- Dual Benefits: Some techniques, like the DIEP or TUG Flap, provide the added aesthetic advantage of a tummy tuck or thigh lift.
- Reduced Risk of Rejection: Since the tissue is from your own body, there is no risk of allergic reaction or rejection.
- Restored Sensation: Certain procedures, such as the DIEP Flap, may allow for nerve reconstruction to restore sensation over time.
Autologous reconstruction is an excellent choice for women who want a holistic solution for breast reconstruction.

What to Expect After Autologous Breast Reconstruction
Recovering from autologous breast reconstruction involves managing symptoms and following your surgeon's instructions. Here’s what to expect during recovery:
- Pain and Swelling: Your surgeon will prescribe medications to control pain, and a pain catheter will numb your abdomen. Swelling in the breast, underarm, and abdomen is normal. Numbness and tightness in the abdomen can last up to twelve months.
- Sensation Changes: You may notice numbness or altered sensation in the reconstructed breast and abdomen. While these changes are often temporary, they can last longer for some patients.
- Healing Timeline: Incisions heal over several weeks. Scars fade gradually, but their appearance depends on your body’s healing process.
- Appointments: Expect to stay in the hospital for two to three days. Your surgeon will see you one week after surgery to monitor healing and remove drains as needed.
General Recovery Timeline
Understanding your recovery timeline helps you plan your return to daily activities:
- Walking and Light Activity: Start walking and climbing stairs as soon as you feel ready, but avoid standing fully upright for the first week.
- Lifting Restrictions: Do not lift anything heavier than ten pounds for the first four weeks.
- Exercise: Avoid heavy exercise, such as running, yoga, or weightlifting, for six weeks. Wait at least eight weeks before starting abdominal exercises.
- Work: Return to work within four to six weeks, depending on your job. Delay returning to jobs that require heavy lifting for eight to twelve weeks.
- Travel: Fly or travel after the first week if you feel comfortable.
- Driving: Do not drive for at least three weeks or while taking pain medications.

Why Choose Park Meadows Cosmetics?
At Park Meadows Cosmetic Surgery, Dr. Christopher Williams and Dr. Jeremy Williams bring exceptional skill to breast reconstruction. Both are board-certified plastic surgeons who trained at the renowned Johns Hopkins Hospital. They specialize in advanced techniques like the DIEP Flap, which uses your own tissue to create realistic results while preserving muscle for faster recovery. Their shared expertise makes them uniquely qualified to handle even the most complex cases and provide outstanding care.
Dr. Christopher Williams has contributed to groundbreaking research and holds patents in tissue engineering, while Dr. Jeremy Williams has published articles, authored book chapters, and presented at national and international conferences on advanced plastic surgery techniques. Their shared knowledge means every patient gets thoughtful care designed just for them. They are well-equipped to help women feel confident and supported before, during, and after their procedures.
Frequently Asked Questions
Prepare by discussing your medical history and goals with your surgeon, stopping smoking if applicable, and following any pre-surgery instructions, such as avoiding certain medications. Eating a healthy diet, staying active, and arranging for help during recovery can also make the process smoother.
Taking care of yourself after surgery will help you have a smooth recovery. Follow these tips to support your healing:
- Diet: Eat small, frequent meals to prevent bloating. Avoid caffeine and chocolate during the first week.
- Wound Care: Empty and record your drain output daily as instructed by your care team. Leave steri-strips and dressings in place until your surgeon removes them at follow-ups.
- Garments: Wear an abdominal binder for three to four weeks to support your healing. Afterward, switch to a control-top garment (e.g., Spanx) if preferred. Avoid compressive bras for three weeks and choose a light camisole for gentle support.
- Bathing: Begin showering forty-eight hours after surgery, keeping water away from your incisions. Avoid submerging in baths, pools, or hot tubs for four to six weeks.
- Medications: Use prescribed pain medications as needed, but avoid aspirin, ibuprofen, and blood thinners for the first week unless advised otherwise. To prevent constipation from pain medications, eat a high-fiber diet or take a stool softener like Colace.
- Sleeping: Sleep in a recliner or elevate your head and knees with pillows for the first two weeks. Avoid sleeping on your stomach for at least four weeks.
- Smoking, Alcohol, and Cannabis: Avoid smoking to support healing and reduce complications. Do not consume alcohol or cannabis while taking pain medications.
- Physical Therapy: Begin gentle range-of-motion exercises during the first two weeks if your surgeon recommends them.
Muscle-sparing techniques like the DIEP Flap preserve abdominal muscles, minimizing long-term weakness. However, older methods like the TRAM Flap may weaken the abdomen, increasing the risk of bulging or hernia. Your surgeon will discuss the best option for your anatomy and goals.
All surgeries will carry some risk. Breast reconstruction surgery involves possible risks such as:
- Surgical Complications: Flap loss, bleeding, infection, pulmonary complications, scarring, seroma (fluid buildup), or abdominal wall hernia.
- Cosmetic Concerns: Asymmetry, size or shape issues, wrinkling, hypertrophic (raised) scarring, or dissatisfaction with results.
- Changes in Sensation: Decreased or altered breast sensation, ranging from increased sensitivity to numbness. These changes can affect sexual response and may be temporary or permanent.
- Pain Management: Mild discomfort is common and managed with prescribed medication. Severe pain that isn’t relieved should be reported to your surgeon immediately.
- Infection: Infections can occur days or weeks after surgery and require prompt treatment to prevent complications.
- Hematoma and Seroma: Hematoma is a collection of blood under the skin, while seroma is fluid buildup under the skin. Smaller collections often resolve naturally, but larger ones may require drainage, leaving a small scar at the drain site.
- Delayed Healing: Slow wound healing or wound separation can occur, especially with factors like smoking, poor nutrition, or a weakened immune system.
Follow your surgeon’s aftercare instructions carefully, including proper wound care and drain management. Avoid strenuous activity or heavy lifting during recovery, as this can increase the risk of fluid buildup. Maintaining a healthy diet and staying hydrated also support proper healing.
- Patients who desire immediate or delayed reconstruction
- Patients with few serious medical problems who desire a breast reconstruction using their own skin and fat
- Patients who want a lower risk of abdominal weakness or bulging
- Patients who have extra tissue, skin, and fat in their lower abdomen and desire a better abdominal contour similar to a tummy tuck
- Patients with the emotional strength and support group to be able to cope with an occasional set-back or loss of the Flap (less than 3% risk of flap loss)
- Patients who understand that extra "investment" in using their own skin and fat is likely to produce a longer-lasting result than an implant-based reconstruction
Breast reconstruction is often covered by insurance under the Women’s Health and Cancer Rights Act (WHCRA), which requires most group health insurance plans to cover reconstruction after a mastectomy. Check with your insurance provider to confirm your specific coverage.
If you are uninsured or have out-of-pocket expenses, financing options may be available. Many practices, including Park Meadows Cosmetic Surgery, partner with healthcare financing companies to offer payment plans to make the procedure more affordable. Give us a call to speak with our office staff about your options.
Autologous Breast Reconstruction Services for Denver and Beyond
To learn more about autologous breast reconstruction, contact our cosmetic surgeons at Park Meadows Cosmetic Surgery in Lone Tree serving Denver and all of Colorado. Schedule a consultation and take a tour of our state-of-the-art facility by calling 303-706-1100 with any questions about our breast reconstruction services.